What is a Bronchoscopy?
So your doctor has scheduled you for a bronchoscopy and you’re thinking, “… A what now?” While the procedure’s name may sound intimidating, fear not: a bronchoscopy is a painless procedure that helps get to the bottom of problems you might be having with your airways. Let’s take a look at just what a bronchoscopy entails, shall we?
What is a Bronchoscopy?
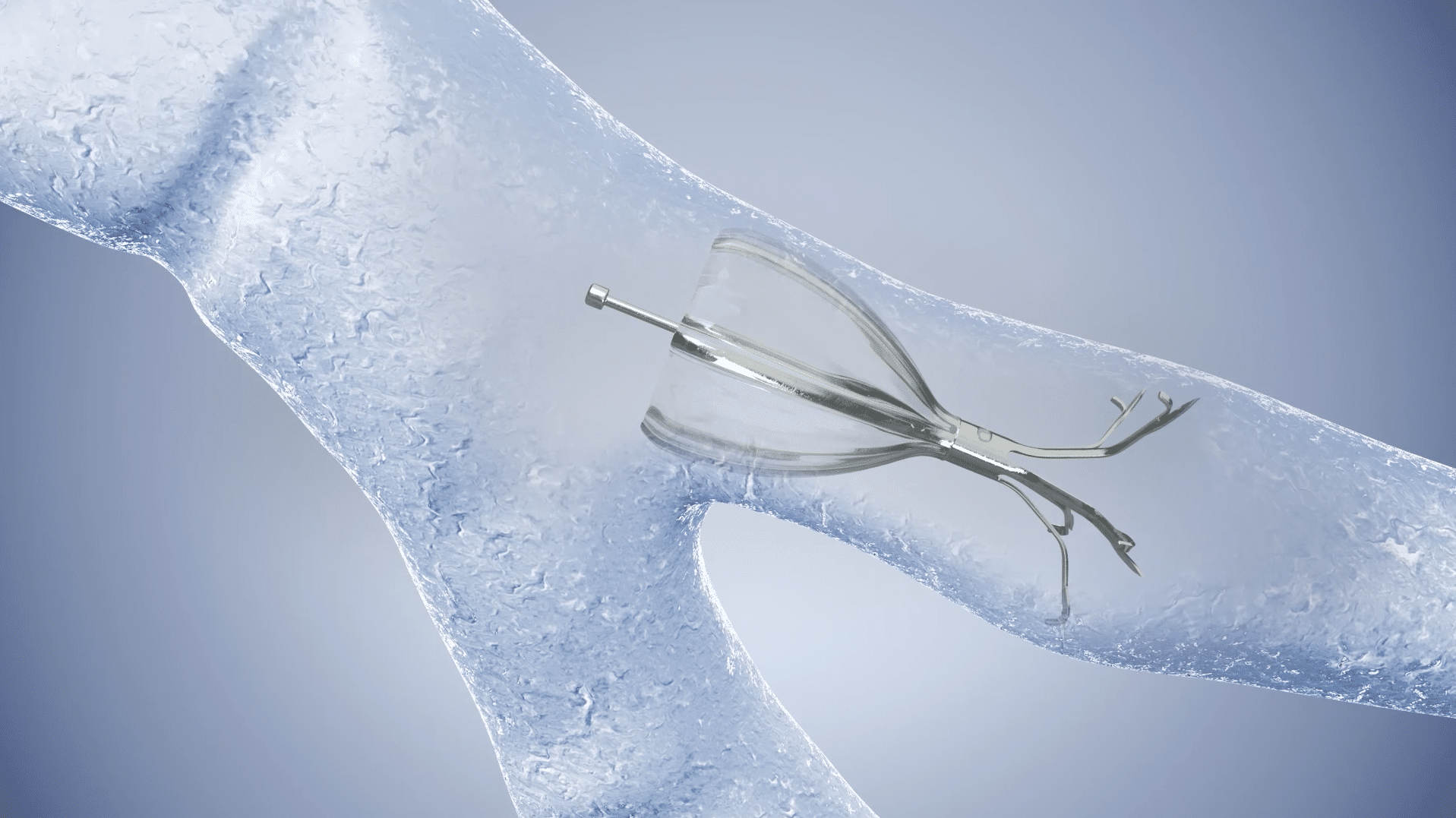
A bronchoscopy is a procedure where your doctor examines your airways using a device called a bronchoscope. A bronchoscope is a thin tube made of a flexible fiber-optic material with a light and a camera on the end that is threaded through your nose/mouth. It lets physicians view all the structures of your respiratory system and will include a clear, precise picture of your lungs.
Does a Bronchoscopy Hurt?
We know, we know… it sounds unpleasant, right? Who wants a tube camera stuffed up their nose? While a bronchoscopy might sound dreadfully painful, the procedure is actually painless and relatively quick. You may experience some discomfort during your bronchoscopy, but your doctor will help talk you through it to make the experience as easy as possible.
Why is a Bronchoscopy Necessary?
Your physician may order a bronchoscopy if you’ve had abnormal chest CT scans or x-rays on which he or she suspects a collapsed lung, infection, potential tumor, or other airway abnormality that needs clearing up. Bronchoscopies are commonly used to diagnose tumors, chronic coughs, infections, and lung disease.
The Different Types of Bronchoscopies
Years ago, there was only one type of bronchoscopy: the routine video bronchoscopy. But just like the tech world, medical advances have come a long way, and now there are a few different types of bronchoscopy procedures. Let’s take a look at each of them, and how they differ from one another.
Routine Video Bronchoscopy
This is the O.G. of the bronchoscopy world and the most standard type of the procedure performed to this day. A routine bronchoscopy is performed using the device we talked about earlier—the bronchoscope. During this test, a specialist (typically a pulmonologist) will insert the bronchoscope through your nose or mouth, down your throat, and into your lungs.
The bronchoscope is very thin and flexible to minimize discomfort. This procedure is typically performed in a hospital or clinic procedure room, and typically lasts 30 to 60 minutes. If you factor in prep and recovery time, you can expect to be at the facility for up to four hours.
Before your bronchoscopy, you may be given medication through an IV to help you relax. Your throat and nose will be sprayed with an anesthetic medicine that helps numb the area to minimize gagging and and unpleasant sensations.
During your procedure, the bronchoscope will travel down your throat and into your lungs to take pictures. Samples of fluid and tissue may be collected by means of devices passed through the bronchoscope—none of this should be painful. After your bronchoscopy, you’ll be monitored for a few hours. Your throat might be numb for a while after the procedure is complete, and until the numbness wears off, you won’t be allowed to eat or drink anything.
You might notice some lingering symptoms of sore throat, cough, muscle aches, or hoarseness in your voice following your bronchoscopy—this is all normal. Call your physician if you experience any of the following symptoms:
- Coughing up more than a tablespoon of blood
- Increase of chest pain
- Trouble breathing
- A fever that lasts more than a day or two
Endobronchial Ultrasound Bronchoscopy (EBUS)
An endobronchial ultrasound bronchoscopy (EBUS, for short) is a procedure used in the diagnosis of infections, lung cancer, and other diseases that cause chest lymph nodes to be enlarged.The EBUS procedure lets your doctor obtain tissue or fluid samples from the lungs and the lymph nodes surrounding them using a technique known as transbronchial needle aspiration (TBNA).
A mediastinoscopy is performed at the same time as the EBUS. This is used to examine the mediastinum—the space behind the breastbone in the middle of the chest. During the procedure, a small incision is made in the neck directly above the breastbone (or sometimes next to it) and a small, thin scope (similar to the bronchoscope, but called a mediascope) is inserted in the incision. This allows access to your lungs and lymph nodes. Next, fluid or tissue is collected via a biopsy.
An EBUS differs from a traditional bronchoscopy is the way patients are prepped for the procedure. An EBUS is typically performed under procedural sedation and local anesthesia, although in certain cases, general anesthesia may be necessary.
After your procedure, you will be monitored until you’re awake enough to leave. A nurse will monitor your breathing rate, blood pressure, and pulse. A chest x-ray may be performed, and you might cough up small amounts of blood.
Since anesthesia is involved in your procedure, you should not drive yourself home—have someone come with you to safely take you home. Ideally, this person should stay with you overnight.
Call your physician immediately if you experience any of the following symptoms post-procedure:
- Coughing up more than a tablespoon of blood
- Chest pains
- Difficulty breathing
Electromagnetic Navigational Bronchoscopy (ENB)
An electromagnetic navigational bronchoscopy may sound like the stuff of science fiction, but we promise it’s real! An electromagnetic navigation bronchoscopy (ENB) is a newer bronchoscopic technique that is primarily used as an early lung cancer detection method.
It uses technology similar to your car’s GPS (yes, seriously!), providing a real-time, 3-D roadmap of your lungs in order to better detect lesions within the lungs—without using surgery. Once a lesion is found, it relays information back to your physician, who can then make an informed decision whether or not to perform a biopsy and form a treatment plan. The ENB test is less invasive than other kinds of lung biopsy procedures.
The ENB procedure process happens in two phases: the planning phase, and the navigation phase.
Planning Phase
During the planning phase of an electromagnetic navigational bronchoscopy, your doctor takes CT scans of your chest and loads them into a program that reconstructs and displays your airways in several 3D images. Your doctor uses these images in order to plan a navigational route and target specific locations within your lungs.
Navigation Phase
After your physician creates a plan, they will then navigate the sensor probe (which is similar to the traditional bronchoscope) to the locations they’ve targeted on the scans. Once the desired location is reached, your doctor locks an extended working channel in place and removes the sensor probe. The working channel then allows access to the targeted lesion for bronchoscopic tools or catheters to take biopsies and samples as needed.
Unlike a traditional bronchoscopy, you will be put under sedation for an ENB. Once sedated, a tube will be placed in your airway. Sedation helps you relax and allows your physician to collect the most accurate reading and biopsy samples as possible.
An electromagnetic navigational bronchoscopy procedure typically takes between 2–2 ½ hours. After it is over, you will go into a recovery room and should be allowed to go home the same day. Since the procedure requires sedation, you will need someone to drive you home and ideally stay the night with you.
Whether you need a routine video bronchoscopy, endobronchial ultrasound bronchoscopy, or an electromagnetic navigational bronchoscopy, The Lung Docs are here. From start to finish, we’re available to answer any questions, ease your fears, and develop the best diagnostic and treatment plan possible with you in mind. To request an appointment, visit our website or give us a call at 423-710-3864.